Use of Antipsychotic Medications in Nursing Homes Declining Regionally
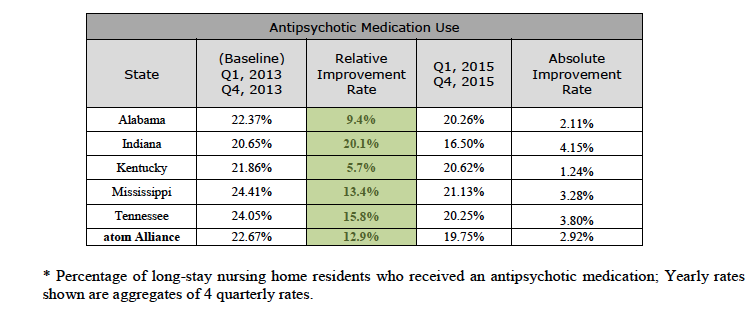
MEMPHIS, TENN. — atom Alliance, a regional Quality Innovation Network-Quality Improvement Organization (QIN-QIO) working under contract to the Centers for Medicare & Medicaid Services (CMS), reports steady progress in its second year of a multi-year effort to reduce unnecessary use of antipsychotic medications among nursing home residents in the states it serves. Across the atom Alliance region, which includes Alabama, Indiana, Kentucky, Mississippi and Tennessee, program efforts resulted in a 12.9 percent relative improvement rate; reducing the unnecessary prescribing and use of antipsychotic medications from 22.67 in 2013 to 19.75 percent in 2015.
High rates of antipsychotic medication use in America’s nursing homes poses a persistent threat to the safety and quality of life of elderly residents, especially those with dementia.
All five atom Alliance states reported improvements in the reduction of antipsychotic medication use. From 2014 to 2015 alone, this improvement positively impacted approximately 2,297 long-term residents in approximately 1,585 nursing homes across the region’s five states. The Alliance’s work in this area is just one part of a larger, longer-term strategy to improve the safety, quality of care and quality of life for nursing home residents.
Team leads with atom Alliance say they’re encouraged by the achievement thus far but will not stop to celebrate current successes for long. Cori Grant, Vice President of Operations at Qsource and Director of the atom Alliance initiative, says atom Alliance continues to work with providers and nursing homes toward loftier goals. “We still have a long way to go and we’re continuing our daily drive toward powerful improvements in this area,” Grant said. “The national program goal is to achieve a 30 percent reduction in the prevalence of antipsychotic medication use in long-term care/nursing home settings by the end of 2016.” That presents a significant opportunity for us to keep moving the needle toward parity with some other states in the country. So we continue to raise that bar and set our sights on higher achievements in healthcare quality and patient outcomes.”
As one of 13 QIN-QIOs working to reduce unnecessary use or misuse of antipsychotic medications throughout the U.S., Virgin Islands and Puerto Rico, the Alliance’s efforts have helped contribute to Medicare’s ability to surpass its 2015 national goal of reducing such usage by 25 percent.
The full report can be found here: Update Report on the Centers for Medicare & Medicaid Services (CMS) National Partnership to Improve Dementia Care in Nursing Homes: 2014 Quarter 2 – 2015 Quarter 3.
Why it Matters
Antipsychotic drugs are sometimes used to treat challenging behaviors associated with dementia, but the FDA warns against using antipsychotics in these patients due to an increased risk of death. Antipsychotics also carry serious risks such as severe, uncontrolled muscle contractions and increased risk of falling. Non-drug treatments are often more effective and safer than antipsychotics.
“We work with providers to identify and implement improvements, on behalf of Medicare, that enhance the lives of nursing home residents,” said Beth Hercher, Quality Improvement Advisor and regional lead for the atom Alliance. “The improvement we’ve achieved in each of our states demonstrates the value of these collaborations at both a statewide and a regional level. This in turn has a positive effect on the nation’s healthcare. We’re quick to share how we’ve accomplished these successes with our peer organizations working across the country.”
atom Alliance serves as the Medicare Quality Innovation Network-Quality Improvement Organization (QIN-QIO). CMS has relied upon coalitions such as atom Alliance to coordinate educational programs, develop tools and resources and conduct outreach to facilities that continue to have high rates of antipsychotic medication use.
Outreach has included the creation of the Leading and Sustaining Systemic Change Collaborative (LSSCC) to produce significant reductions in each of the 950 Alliance-recruited facilities. Strategies implemented included regular chart reviews to ensure proper medication use, weekly psychiatric evaluations, routine multidisciplinary meetings and ongoing education on proper use and risks of antipsychotic medications.
“We also work closely with state and national partners to share and develop learning opportunities for widespread change,” said Hercher. “We partnered with the Tennessee Eden Alternative Coalition to highlight the Reframing Dementia training that explores the art of building meaningful relationships as the fundamental building block of care.We also partnered with the Vanderbilt Center on Quality Aging to host a six-part Webinar series focusing on addressing barriers to change.”
Reduction of Nursing Home Antipsychotic Medication Use by Each atom Alliance State:
IND. — Prevalence of antipsychotic medication use among Indiana’s nursing home residents was reduced from 20.65 percent in 2013 to 16.5 percent in 2015 resulting in a relative improvement rate of more than 20 percent. These improvement efforts positively impacted more than 850 residents in Indiana nursing homes.
KENT. — Prevalence of antipsychotic medication use in nursing home residents was reduced from 21.86 percent in 2013 to 20.62 percent in 2015 resulting in a relative improvement rate of nearly six percent. These improvement efforts positively impacted more than 120 residents in Kentucky nursing homes.
TENN. — Prevalence of antipsychotic medication use in nursing home residents was reduced from 24.05 percent in 2013 to 20.25 percent in 2015 resulting in a relative improvement rate of nearly 16 percent. These improvement efforts positively impacted more than 680 residents in Tennessee nursing homes.
MISS. — Prevalence of antipsychotic medication use in nursing home residents was reduced from 24.41 percent in 2013 to 21.13 percent in 2015 resulting in a relative improvement rate of 13.43 percent. These improvement efforts positively impacted more than 250 residents in Mississippi nursing homes.
ALA. — Prevalence of antipsychotic medication use in nursing home residents was reduced from 22.37 percent in 2013 to 20.26 percent in 2015 resulting in a 9.4 percent relative improvement rate. These improvement efforts positively impacted more than 400 residents in Alabama nursing homes.
For information visit www.atomAlliance.org.
###
About atom Alliance
atom Alliance is a five-year, five-state initiative to ignite powerful and sustainable change in healthcare quality. Formed as a partnership between three leading healthcare consultancies, atom Alliance is working under contract to THE CENTERS for MEDICARE & MEDICAID SERVICES (CMS) to improve quality and achieve better outcomes in health and healthcare and at lower costs for the patients and communities we serve. Through atom Alliance, AQAF in Alabama, IQH in Mississippi and Qsource in Indiana, Kentucky and Tennessee are carrying out an exciting strategic plan, with programs in place to convene, teach and inform healthcare providers, engage and empower patients, and inspire, share knowledge and spread best practices with communities across the entire healthcare continuum.
Resource:



