
Rural Mississippi Community Empowers Pharmacists and Reduces Hospital Readmissions
People with complex medication routines who are admitted to the hospital are at a higher risk for readmission due to several factors, including gaps in the continuity of care. Care transitions can be difficult and as patients transition from the hospital setting to home, they are particularly vulnerable to medical error, especially to adverse drug events (ADEs).
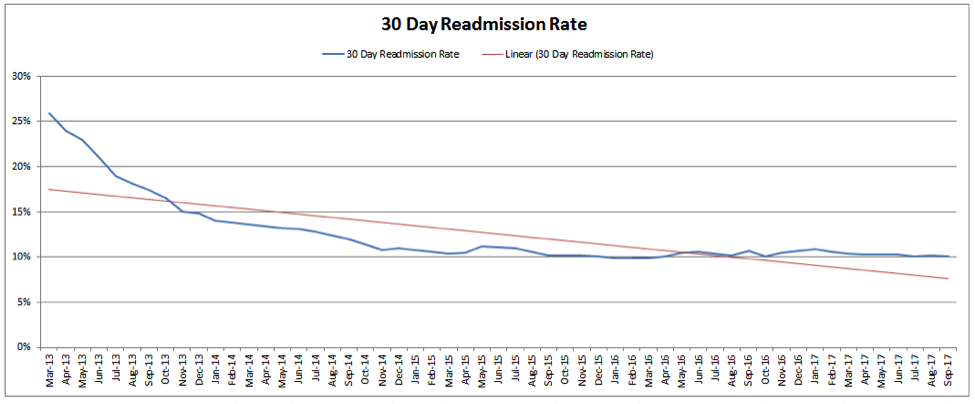
The Three Rivers Healthcare Coalition in northeast Mississippi saw this as an opportunity for improvement in their rural community. Working with Qsource quality improvement advisors and the local hospital, the Coalition implemented pharmacy-directed transitional care in 2013. As a result, the rate of hospital readmissions for patients receiving this intervention has dropped from 26 percent to about 10 percent in five years.
“When a person is discharged from the hospital, it’s critical that they take the right medications at the right times to avoid complications and being readmitted. So it makes perfect sense to put pharmacists in charge of that transition,” said Qsource quality improvement advisor, Mary Helen Conner, PhD.
According to the Centers for Medicare & Medicaid Services (CMS), the average 30-day readmission rate in the United States is about 16 percent. The American Journal of Pharmaceutical Education reports nearly two-thirds of post-discharge adverse events are medication related. Twenty-nine percent of these ADEs are serious or life-threatening, sometimes resulting in emergency department visits and unscheduled hospital admissions. However, as many as 60 percent of post-discharge ADEs could be prevented or improved with intervention by health professionals at or shortly after discharge.
The designated pharmacist receives a daily report of Medicare beneficiaries who have been discharged from the local hospital. The clinical pharmacist calls the patients within two days to go over their discharge instructions and schedule a follow-up appointment with their physician. The initial follow-up appointment is scheduled within 14 days of hospital discharge.
“Based upon CMS readmission data, it’s important that providers see patients quickly after discharge to prevent unnecessary readmissions,” said pharmacist, Dr. James Taylor, from the Family Medicine Residency Center in Tupelo. “Our goal is to have them seen during the first week post-discharge, but this is not always possible for every patient.”
Clinical pharmacists discuss medication reconciliation, medication therapy management and preventive care services like immunizations with the patient and make notes for their physician to discuss during follow-up appointments. They also track data for the intervention, including each time they contacted the patient, if the patient kept their appointments, and if/when the patient was readmitted to the hospital.
Measuring Success
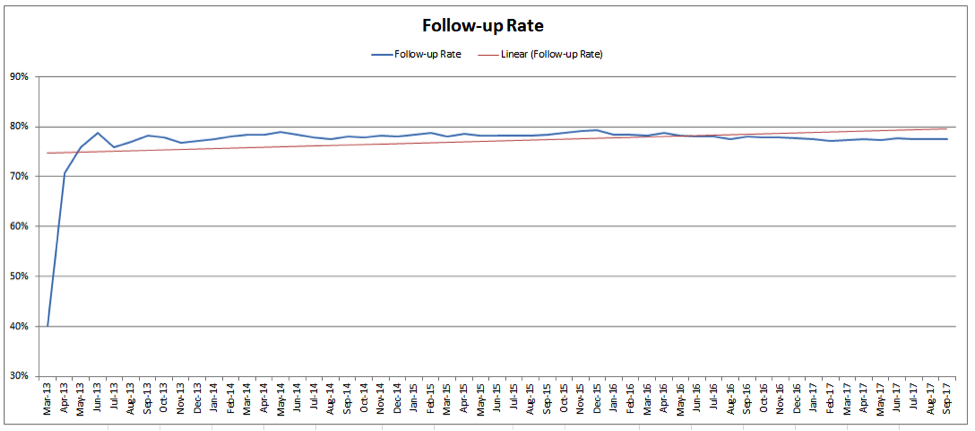
Qsource analysts measure the pharmacist-directed transitional care intervention by the follow-up rate and the 30-day readmission rate. The follow-up rate shows the Medicare patients who spoke with the clinic contact, scheduled their follow-up appointment and attended that appointment, as opposed to not showing up for that critical first appointment after discharge. After beginning this targeted intervention, nearly 80 percent of the patients helped by the clinical pharmacist show up for their follow-up appointment.
“Getting patients to show up for that follow-up appointment is key to keeping them on track and out of the hospital,” Conner said. “This intervention places an emphasis on that follow-up visit, making it very effective.”
The 30-day readmission rate shows the Medicare patients who spoke with the clinical pharmacist, scheduled their follow-up appointment and were readmitted to the hospital within 30 days of being discharged initially. The Coalition has seen an almost 60 percent reduction in these types of readmissions since beginning the intervention in early 2013.
Looking Forward
The Coalition plans to continue this intervention in northeast Mississippi. Conner has recommended the pharmacist/resident call a second time after the follow-up visit, particularly for those patients identified for high readmissions, for example, patients with alcohol misuse disorder or those that are non-compliant.
“We are thrilled with not only the success of this intervention but the fact that they have been able to maintain their success for several years by putting pharmacists at the forefront of care transitions,” Conner added. “It’s exciting to be able to impact these people with Medicare and avoid unnecessary hospital stays for almost 1,000 Mississippians so far.”
For more about Qsource and the care transitions work we do with communities, visit .
 Skip to main content
Skip to main content

