Facility Exceeds National AP Reduction Goal
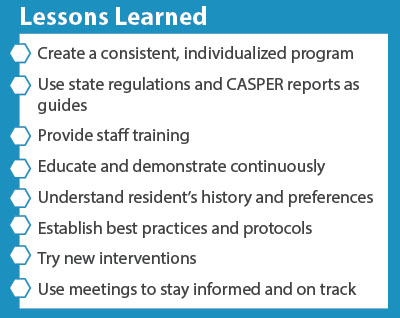
They accomplished this by developing a consistent and individualized gradual dose reduction (GDR) program, using state regulations and the CASPER report as guides.
Nursing Administration, headed by Assistant Director of Nursing, Renea Standridge, led the change, accompanied by all nursing staff and pharmacy consultants.
First, they educated themselves on how to best approach the project and secured involvement and buy-in from the Medical Director and Certified Registered Nurse Practitioner.
They realized that dementia training would be essential and started a campaign that involved nursing, certified nursing assistants (CNAs) and activities staff, eventually mandating dementia training for all employees.
The effort faced some resistance. Families were concerned about GDRs with the intent to discontinue the medication. Staff feared that some residents wouldn’t function well without these medications.
Standridge and her team overcame these concerns through education and demonstration.
They educated family members individually and unit managers about state and national regulations, dementia and dementia-related behaviors. Nursing staff received dementia training, including Hand in Hand, Teepa Snow and Virtual Dementia Tours.
They also gathered as much personal information as possible on a resident before they attempted GDR.
“Learn their habits, hobbies, likes and dislikes,” Standridge said. “Also find out the history of how and why the antipsychotic was started.”
Eventually, they established a protocol for addressing behaviors in residents with dementia by using an AP worksheet.
These strategies worked. While the national goal for AP reduction was 15 percent, Hanceville Nursing and Rehab Center exceeded it by reducing AP drug use to 13.5 percent.
Standridge shared a story about one resident.
“A 73-year-old female with a diagnosis of dementia with behavior disturbance was receiving Risperdal in November 2012 for fixed false beliefs and hallucinations,” McClellan said. “We had several failed GDRs documented. After attending a workshop sponsored by Alabama Quality Assurance Foundation (AQAF) about music therapy, we started using headphones with music and attempted GDRs again; this time, with success. She was completely discontinued from Risperdal and received no other antipsychotic by June 2013.”
With the reduction came several benefits that improved the quality of life for the residents. The side effects of sedation, which contributed to nutritional deficiencies and fall risk, decreased. Weight loss decreased by 30 percent and falls with major injuries by 23 percent.
Negative behaviors also did not increase. In fact, trips to geri-psych were reduced.
Relationships between caregivers and residents improved as well. CNAs have been able to get to know their residents better because the residents have become involved in activities.
To sustain this gain, Standridge holds quarterly meetings with RN unit managers to review all residents on APs to assess GDR. They continue educating staff with annual Hand in Hand training and monitoring data from CASPER, Advancing Excellence and NADONA LTC.
They also continue working with AQAF, now part of the five-state atom Alliance, a five-year initiative to ignite powerful and sustainable change in healthcare quality.

Preview: Facility Exceeds National AP Reduction Goal - AL Success Story
Download
722.63 KB | Last Updated: February 6, 2015

14.SS.AL.C2.09.002


